[ad_1]
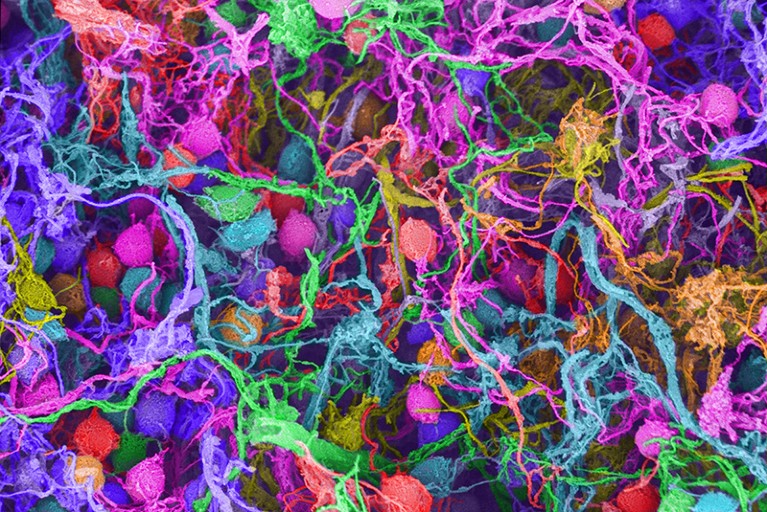
Scanning electron micrograph of human brain cells — can psychedelics rewire them safely?Credit: Ted Kinsman/SPL
Psychedelic drugs can cause lasting effects on the brain. Just a single dose of these mind-altering substances can spur neurons to grow new offshoots called dendritic trees and branches that engage with their neighbours, creating elaborate networks of interconnected brain cells. This rewiring of neural circuitry helps to boost mood, combat depression and increase overall feelings of wellness. It can happen within days, and the benefits can last for months.
Chemical neuroscientist David Olson demonstrated1 this in 2018. Working on rats, fruit flies and zebrafish, he and his colleagues at the University of California, Davis, found that a variety of psychotropic medicines — including hallucinogenic agents LSD and DMT, as well as stimulants such as MDMA (commonly known as ecstasy) — rapidly produce these changes in brain architecture.
Part of Nature Outlook: Psychedelic medicine
But these drugs come with plenty of downsides. They can cause life-threatening heart problems. Their perception-distorting effects make them ill-suited for individuals who might not respond well to hallucinations or other sensory alterations. And the need to administer the treatments under clinical supervision, often alongside psychotherapy sessions, can drive up costs and limit access for people who might otherwise benefit from the drugs’ ability to rewire the brain.
Hoping to find safer, more scalable alternatives, Olson started looking for compounds that pack the plasticity-inducing punch of true psychedelics but are free from their other-worldly experiences. He turned to Reddit and other online forums, searching for molecules that recreational-drug enthusiasts had already created but deemed to be failures — “psychedelic duds”, as Olson puts it. These agents lacked the hallucinatory powers their creators had been hoping for, but Olson found that many of them could trigger neuronal growth nonetheless.
Olson then tasked members of his lab group with synthesizing psychedelic-like molecules of their own. These efforts yielded tweaked versions of DMT2 (the active chemical in ayahuasca tea) and ibogaine3 (a drug harvested from the roots of an African shrub) that had improved safety and reduced hallucinogenic properties. Olson now plans to develop these compounds through a start-up biotechnology company he co-founded called Delix Therapeutics, based in Boston, Massachusetts.
Olson is not alone. Drawing inspiration from psychoactive medicines, a growing number of biotechnology companies and academic researchers now aim to improve on what nature and decades-old drug-discovery efforts have to offer. “The goal is really to find better ways — more efficient and effective ways — to treat depression” and other types of mental illness, says Natalie Hesselgrave, a neuroscientist at Yale School of Medicine in New Haven, Connecticut.
Some are making minor modifications to existing agents, aiming to fine-tune the speed of onset and duration of drug activity for a more consistent experience. But many are developing entirely new chemical entities with the goal of laying the foundation for a new generation of brain-restructuring therapeutics to treat mental illness.
“This whole field has exploded,” says John McCorvy, a chemical neuropharmacologist at the Medical College of Wisconsin in Milwaukee. He works with companies including COMPASS Pathways, based in Altrincham, UK, and Bright Minds Biosciences in New York City to screen new psychedelic-inspired drugs. “We are hungry for new and exciting compounds,” he adds.
The creation of non-hallucinogenic psychedelic analogues remains a top priority for the industry. But many researchers are sceptical that the consciousness-expanding effects of psychedelic medicines can easily be decoupled from their therapeutic benefits. “I’m not convinced that mouse pharmacology is easily translated to human pharmacology, at least in this realm,” says David Nichols, a medicinal chemist at the University of North Carolina (UNC) at Chapel Hill and professor emeritus at Purdue University in West Lafayette, Indiana. “There’s a cognitive component that I think is important for the therapy” in a lot of mental-health conditions, he adds, referring to the types of out-of-body, mystical experiences that have been shown to help people who have existential distress or substance-use disorders. “I think you really need that.”
That assertion is now being put to the test, with several non-hallucinogenic drugs — including two ibogaine derivatives and two LSD analogues — now in or nearing their first human trials. These projects could address the central question of whether those altered states of consciousness are a necessary part of the therapeutic enterprise. “We’ll never know for certain until it’s tested in people,” Olson says.
Property search
The pharmaceutical industry’s interest in psychedelics-inspired drugs goes back a long way. Scientists at Merck in Darmstadt, Germany, discovered MDMA more than 100 years ago. A couple of decades later, the chemist Albert Hofmann first synthesized LSD in 1938 while working at Sandoz (now part of Novartis) in Basel, Switzerland. In both cases, however, the compounds were swiftly abandoned as therapeutic candidates. At the time, Merck and Sandoz were focused on treating blood disorders, not mental illness, so the psychedelic or stimulant effects of these agents were seen as liabilities, not properties to be harnessed for therapeutic gain.
For decades, anyone wanting to investigate psychedelic medicine for mental-health conditions was stigmatized and faced legal restrictions. Few chemists or pharmacologists dared to develop compounds with psychedelic properties. “You couldn’t get any funding,” says Nichols, one of the few scientists who did get government research grants on the topic. “It was the kiss of death back then,” he says.
That’s no longer the case. Thanks to a better understanding of how psychotropic medicines work in the brain, and buoyed by clinical data showing profound benefits of taking drugs such as psilocybin for depression, or MDMA for post-traumatic stress disorder, these molecules have re-entered the medical mainstream.
The US National Institutes of Health now funds multiple research teams, including Olson’s, to create psychedelic analogues. And in 2020, the country’s Defense Advanced Research Projects Agency (DARPA) earmarked a whopping US$27 million for research into new chemicals directed at some of the brain receptors that psychedelics use. “There’s a huge space for innovation,” says Tristan McClure-Begley, who is a former programme manager for DARPA who now leads the Integrative Neuroscience Branch at the US National Institute on Drug Abuse in Bethesda, Maryland.
Bryan Roth is a molecular pharmacologist at UNC who is leading the DARPA-backed project. For years, he has been studying how a protein found on neurons is central to the activity of drugs such as LSD. Indeed, a psychedelic is now defined as any drug that works by stimulating this protein, a serotonin receptor known as the 5-hydroxytryptamine 2A (5-HT2A) receptor.
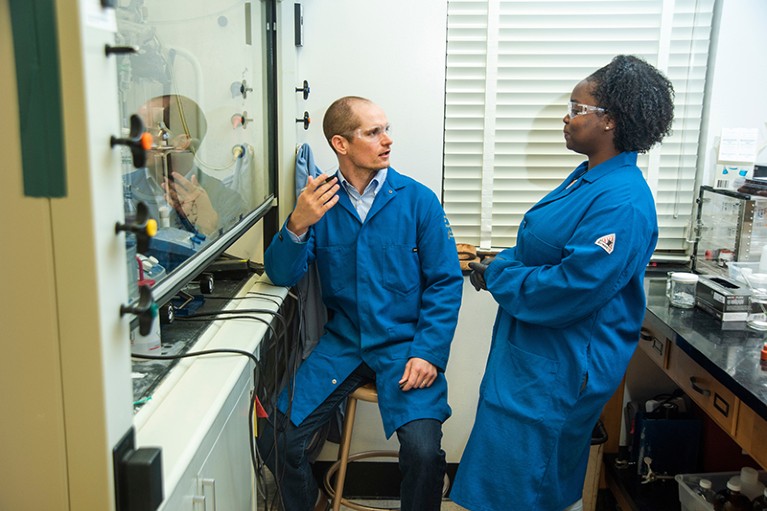
David Olson talks to a student about his work to find non-hallucinogenic psychedelic drugs.Credit: UC Davis
But psychedelics such as LSD, psilocybin and DMT — a class of molecules known as tryptamines — also hit many other brain receptors. In the parlance of pharmacology, that makes them ‘dirty’ drugs, and complicates efforts to pin down exactly how they work. Researchers don’t really know whether the activation of multiple serotonin receptors contributes to their therapeutic effect. But it’s clear that engaging receptors such as 5-HT2B, a protein related to 5-HT2A, increases the risk of drug-induced toxicity.
Roth’s task has been to find compounds that target the 5-HT2A receptor and little else, to understand what drives the therapeutic effects of psychedelics and to create safer potential drug candidates. His team started by virtually screening billions of drug-like compounds, looking for molecular structures predicted to be selective for just this one receptor. The search yielded some 70,000 chemical scaffolds4 — “enough new chemical matter to keep all of the medicinal chemists in the world busy for many years”, Roth says.
The researchers have begun to investigate some of these in more detail. One type of molecule, for example, seems to cause no hallucinogenic activity but still exerts anti-depressant and anti-anxiety effects in mice. Roth and his colleagues now hope to select a drug candidate for evaluation in people.
No other research effort into psychedelics has yielded anything nearly so receptor specific. Perhaps this is not surprising, given that most of the others centre around finding derivatives of known psychotropic agents, all of which have complex pharmacological properties. The predominant strategy, as Peter Facchini explains, is to start with an existing medicine and “then find ways of improving it”.
Facchini is a plant biochemist at the University of Calgary in Canada and chief innovation officer at Enveric Biosciences — a company based in Naples, Florida, that has developed a collection of nearly 1,000 tryptamine derivatives. Facchini calls this the Psybrary. “Now, we’re looking for the proper drug that has the right pharmacologic properties,” Facchini says.“It’s a long-overdue return to these classes of compounds.”
Safety first
Some companies are prioritizing safety in their search, given that many psychedelics and stimulants can cause cardiac anomalies. For example, EmpathBio, a subsidiary of Berlin-based atai Life Sciences, plans to start human testing later this year with a proprietary derivative of MDMA that avoids interactions with certain receptors linked to drug-induced increases in heart rate and blood pressure. “You should be able get better safety by mitigating some of that pharmacology,” says atai’s co-founder and chief scientific officer Srinivas Rao.
Others are trying to take hallucinations and other sensory disturbances out of the equation — and that means adjusting not just which receptors become activated, but also how downstream signalling cascades play out. Earlier this year, a research team from China, led by medicinal chemist Jianjun Cheng at ShanghaiTech University and structural biologist Sheng Wang at the Shanghai Institute of Biochemistry and Cell Biology, showed that a specific binding mode of psychedelics preferentially promotes one of the 5-HT2A receptor’s two main signalling pathways. Harnessing this biased signalling helped the researchers to design psychedelic-like agents with antidepressant potential but no hallucinogenic effects5. According to Cheng, the team is now optimizing the compounds for potential human therapeutic use.
Dina Burkitbayeva, co-founder and general partner at PsyMed Ventures, an investment fund based in San Francisco, California, thinks this search for new psychedelic-like molecules is a double-edged sword. From a business perspective, she says, “you’re really trying to balance two things”. New chemical matter is easier to patent-protect, and hence could yield greater profits. A well-designed drug might offer a better therapy, too.
But that outcome is highly uncertain. Developing any novel therapeutic is inherently risky, because most new drug candidates fail in clinical trials. What’s more, it remains an open question whether taking the trip out of psychedelic drugs will still yield an effective therapy.
That’s why PsyMed, along with other investors in the field, such as Vine Ventures, Palo Santo and the Noetic Fund, are hedging their bets. On the speculative front, they are backing start-ups working on the next generation of psychedelic-adjacent medicines. But they are also funding companies with proprietary formulations of psilocybin and MDMA — psychotropic medicines that already have proven records of clinical success.
To enable that kind of discovery, some researchers are taking a function-oriented approach to chemical synthesis. In Olson’s lab, for example, a team led by neuroscientist Lindsay Cameron systematically deleted each of the three main structural elements found in ibogaine to identify which parts were needed for neuron growth and which parts could be safely discarded. That effort yielded an analogue that was easier to synthesize and had all the desirable properties of ibogaine but lacked features that made the compound more likely to cause heart problems. Then it was simply a matter of swapping around a pair of chemical side chains, and the researchers had their non-hallucinogenic variant3. “All the pieces fell into place,” recalls Cameron, who is now at Stanford University in California. “It was beautiful.”
To identify similar molecules, Olson teamed up with Lin Tian, a neuroengineer also at the University of California, Davis, to develop a cell-imaging tool called psychLight that can discriminate between compounds that have hallucinogenic properties and those that do not6. Thinking more broadly about the plasticity-producing benefits of psychedelics, and not just their consciousness-altering traits, other research groups have fashioned biosensor platforms to determine whether drugs have the desired brain-rewiring potential.
For instance, neuroengineer Alex Kwan at Cornell University in Ithaca, New York, and his colleagues devised a system7 for imaging the entire mouse brain and mapping the expression of c-Fos, a protein found in actively growing neurons. Kwan’s group used ketamine and psilocybin to establish a blueprint of drug-induced c-Fos expression against which other researchers can benchmark their own therapeutic candidates — allowing them to, as Kwan puts it, “look for plasticity across the whole brain”.
Neuropharmacologist Javier González Maeso has also discovered a molecular signature consistent with induced neuroplasticity. Focusing on the frontal cortex, a brain region that is implicated in mood and anxiety disorders, he and his team at the Virginia Commonwealth University School of Medicine in Richmond identified8 a pattern of genetic and epigenetic changes linked to the enhanced density of dendritic connections in mice after treatment with a psychedelic agent called DOI.
In unpublished follow-up work, the team repeated the experiment using LSD and, according to González Maeso, “it did something similar”. Now, he says, the genetic signature “can be used as a screening tool” to discover new plasticity-promoting agents.
A little less hallucination
Many of those who study psychedelic drugs do not see the issue of hallucinations as an all-or-nothing proposition. Hooshmand Sheshbaradaran, chief operating officer of BetterLife Pharma in Vancouver, Canada, thinks that the acceptable level of hallucinogenic effects might depend on the therapeutic setting.
Non-hallucinogenic agents such as BetterLife’s LSD derivative, which is due to enter human testing in 2023, might, for instance, be used at home by people with mild depression. By contrast, he says, the people who were most ill and hospitalized with treatment-resistant depression could be given psychedelics with more-potent cognitive effects under controlled conditions.
In some cases, simply minimizing the trip might be enough. “You could, for example, engineer something that has a short psychedelic effect but a longer neuroplastic effect,” Rao says.
More from Nature Outlooks
“It’s really about trying to fine-tune where that therapeutic window is,” adds Jackie von Salm, co-founder and chief scientific officer of Psilera, a biotech company based in Tampa, Florida, that is developing medicines based on DMT and psilocybin.
At Gilgamesh Pharmaceuticals in New York City, a company spun off from Dalibor Sames’s neurochemistry lab at Columbia University, researchers are working on an antidepressant built on a tryptamine template. One of the company’s first products to enter human testing will be a rapid-acting psychedelic that will still induce mind-bending effects, but the trip should last only about one hour, not the 6–12 hours typical with psilocybin or LSD.
“It will be much less resource intensive, in terms of therapists’ time and burden on the health-care system,” says the company’s co-founder and head of chemistry, Andrew Kruegel. Gilgamesh is also developing a rapid-acting derivative of ketamine that can be taken orally with fewer dissociative effects, as well as analogues of ibogaine that have improved cardiac safety.
Kruegel thinks these less-hallucinogenic analogues will eventually complement or even supplant the drugs on which their chemical structures are based. “We see these being the ultimate preferred choice among people who are going to be using these therapies given the efficacy, safety or convenience improvements we’ve introduced,” he says. “Hopefully, these will be therapies that can actually be delivered to millions of people, as opposed to a very limited group.”
[ad_2]
Source link