[ad_1]

In the United States, people from minority ethnic groups with diabetes have higher rates of kidney disease than white people with diabetes.Credit: Gary Friedman/Los Angeles Times via Getty
Nephrologist C. Elena Cervantes routinely encounters racial and economic disparities among her patients with chronic kidney disease (CKD). Most of them are Black or Hispanic, says Cervantes, at Johns Hopkins Medicine in Baltimore, Maryland. They live in poor, medically under-served neighbourhoods, and have type 2 diabetes — the top risk factor for CKD. Cervantes is from Ecuador, and says that the people with kidney disease she saw during her years as a medical student in Latin America were in similar circumstances. “They were also poor and frequently delayed treatment until they felt they could no longer continue working,” Cervantes says. “By the time we diagnosed them, they typically needed dialysis.”
Roughly 80% of people with diabetes — and 75% of the 500 million people with CKD around the world — reside in low- and middle-income countries (LMICs). And in the United States, Black, Hispanic, American Indian, Alaska Native and Pacific Islander people with diabetes develop CKD at rates that are significantly higher than those of white people, according to one study1 (see ‘A disproportionate crisis’). “CKD is the most serious and most common complication of diabetes,” says the study’s lead author, Katherine Tuttle, a nephrologist at the University of Washington in Seattle. And as diabetes cases increase globally, she adds, the accompanying spike in CKD among some groups signals a worrying trend.
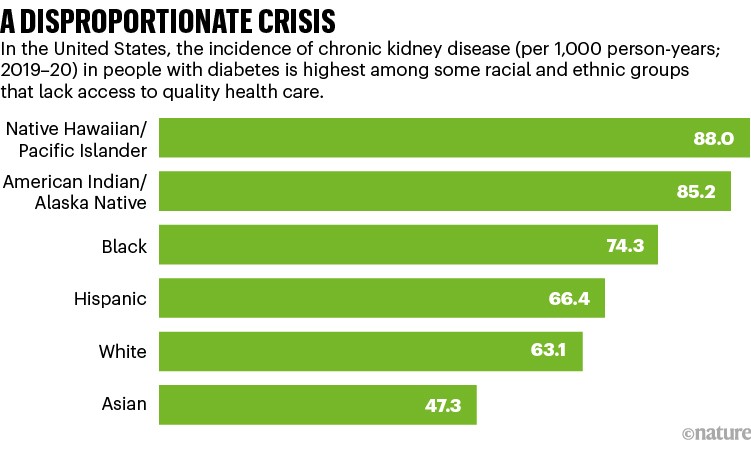
Source: Ref. 1
Diabetes leads to CKD by an insidious route and is often not detected in its early stages. The kidneys have evolved to funnel waste into urine while returning essential proteins, minerals and electrolytes to the bloodstream. But high levels of blood sugar in people with diabetes damage the kidney’s functional units, called nephrons. Every kidney contains roughly 1.5 million nephrons, and as these structures are lost to diabetes, CKD takes hold. The onset of disease is asymptomatic at first — most people with diabetes are unaware that they have kidney disease until they develop fatigue, swelling and cramps — symptoms that often lead to a late-stage diagnosis. Meanwhile, CKD elevates the risk of deadly complications, including infections, pneumonia and sepsis, in addition to kidney failure. By the time CKD reaches stage 3 — moderate kidney damage — “the mortality rate is comparable to other conditions well-recognized as likely to be fatal, such as many common types of cancer”, Tuttle says.
Early detection
Scientists are now working to reduce the global burden of diabetes-associated CKD — a goal that depends above all else on identifying the condition early, when treatments can slow its progression more effectively. But in low-income settings, early screening for CKD is uncommon. Untreated type 1 diabetes, which occurs most often in children and adolescents, generally progresses to kidney disease in two to five years, after which renal function should be assessed annually. Type 2 diabetes typically develops later in life and is often accompanied by poorly controlled blood sugar and high blood pressure. Clinical guidelines recommend immediate CKD screening for people who have been diagnosed with type 2 diabetes. Cervantes and her co-authors have reported2, however, that late referrals for kidney-function screening in LMICs leave many people with diabetes vulnerable to end-stage kidney disease (ESKD).
Part of Nature Outlook: Chronic kidney disease
Among the various barriers to early CKD detection, the authors cited insufficient awareness of kidney disease among people with diabetes and physicians, high screening costs and scarce laboratory facilities. To keep kidney disease at bay, people with diabetes need to maintain their blood sugar at healthy levels. Yet barely 30% of people with diabetes in LMICs receive treatment, Cervantes says, in part because the cost of standard therapies, such as metformin and insulin, is out of reach of many people. That’s also true of drugs used for treating hypertension, which is the second leading cause of CKD. “This was shocking,” says Cervantes. Diabetes and hypertension must be treated to head off renal failure in people with diabetic kidney disease. Yet these basic underlying risk factors “are unaddressed for most populations”, Cervantes says.
Even in wealthy countries, diabetes is much more likely to lead to kidney disease in low-income populations than in more well-off ones. According to another study by Tuttle and her colleagues, fewer than half of all people with diabetes in the United States are routinely screened and monitored for kidney disease3. Key impediments, the authors say, are the complexities and time constraints involved in treating CKD. Commonly used agents, including angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs) and mineralocorticoid receptor antagonists, require intensive dose monitoring to limit the risk of elevated blood potassium levels.
Physicians can be reluctant to prescribe these drugs and people can be unwilling to take them. Working out these details can require multiple visits to the clinic. High out-of-pocket costs and low reimbursement rates pose further barriers to treatment, especially among those without sufficient health insurance to cover the cost. Tuttle and her co-authors called for a reduction in disparities in access to drugs; not just to newer drugs such as sodium-glucose cotransporter-2 (SGLT2) inhibitors that cost between US$320 and $580 per month, but also to more standard therapies, such as ACE inhibitors and ARBs, the use of which is also low among people with low incomes.
Better outcomes with quality care
When people from different groups in the population have equal access to high-quality diabetes care, however, disparities in functional kidney outcomes start to disappear, Tuttle says. She cites a steep reduction in ESKD rates achieved by Alaska Native and American Indian groups treated for diabetes by the US Indian Health Service (IHS). In 1996, ESKD rates among these groups were almost five times higher than those among white people with diabetes. By 2013, the rates had decreased by 54%4. Andrew Narva, a nephrologist and chief consultant to the IHS Kidney Disease Program based in Washington DC, attributes that success to what he describes as an interdisciplinary approach to community-based care. The basic strategies included routine CKD screening, an expanded focus on glucose and blood-pressure control, and the use of ACE inhibitors and ARBs where necessary. “It was really about successfully implementing relatively simple interventions effectively and sustainably,” Narva says.
Research has also shown that when treated for diabetes in clinical trials, white people and those from minority ethnic groups achieve similar kidney-function outcomes. The Action to Control Cardiovascular Risk in Diabetes (ACCORD) clinical trial, for instance, tested drugs for blood-sugar and blood-pressure control in Black and white people with diabetes. An analysis5 of the trial results by Tamara Isakova, a nephrologist at Northwestern University’s Feinberg School of Medicine in Chicago, Illinois, and her colleagues showed that Black people ultimately ended up with a lower incidence of CKD than did white people. To Isakova, the conclusion is clear: using the same interventions with Black people and white people makes it possible to “prevent some of the CKD disparities that we see out in the community”.
More from Nature Outlooks
But Jenna Norton, an epidemiologist at the National Institute of Diabetes and Digestive and Kidney Diseases in Bethesda, Maryland, argues that to fully address racial and ethnic disparities in CKD, researchers should also examine the upstream social determinants that drive up disease rates in the first place. People living in low-income areas, Norton says, typically have poor access to medical services, and experience food insecurity. “If you have to take buses to get to a grocery store, then that mediates your ability to maintain a healthy diet for yourself and your family.”
Poor maternal nutrition might also predispose children to diabetes and CKD risk later in life, argues Ann Bullock, a family physician and a member of the Minnesota Chippewa Tribe who retired from the IHS in 2021. Diets high in fat and carbohydrates, she says, as well as maternal stress during pregnancy, can alter a child’s metabolic profiles, resulting in reduced numbers of nephrons and insulin-secreting β cells. “Poverty is endemic in Indian reservations,” Bullock says. “And when you no longer have access to the healthy foods you used to have, that sets up the perfect storm for chronic diseases passed through generations.” The IHS’s diabetes programme works to improve nutrition on reservations, in part by supplying grant funds for community vegetable gardens.
Research on the root causes of CKD present difficult challenges. “Everyone would agree that social determinants are major contributors to overall health,” says Chi Chu, a nephrologist at the University of California, San Francisco. “The problem is that they are not well measured in populations. So, it’s hard to say that changing a particular determinant leads to an improved outcome.” Still, Chu adds that in light of how social factors influence the prevalence of diabetes and kidney disease, efforts limited to improving health-care delivery “may not be enough to eliminate disparities”.
Meanwhile, at Johns Hopkins, Cervantes continues to grapple with the problems of treating a mostly minority-ethnic population. Although her patients should receive up-to-date medications, such as SGLT2 inhibitors, which produce better outcomes than standard drugs, costs are a constant issue, she says, and so are the challenges of frequent monitoring for complications. Similar to the people she saw while at medical school, most of her patients are diagnosed with advanced disease, which is harder to manage, and clinicians are often hesitant to initiate therapy with the best available drugs. “We’re not establishing care early enough,” she says. “Despite all the new trials showing benefits with new agents, there’s still room for improvements.”
[ad_2]
Source link