Supported by Science
Ask Gerda: Are There Side Effects from MRI Contrast Dyes?
Ask Gerda: Are There Side Effects
from MRI Contrast Dyes?
April 21, 2022

Gerda Endemann, our senior director of science and research, has a BS in nutrition from UC Berkeley, a PhD in nutritional biochemistry from MIT, and a passion for cherry-picking from our wellness shop. She spends a lot of her time interpreting research—established and emerging. You’ll find some of her deep dives into health conditions in our growing library of articles called goop PhD. You can send your own questions for Gerda to editorial@goop.com..
Dear goop, I think I’m allergic to the dye I was injected with when I had two MRIs. Since then, I’ve had hives, brain fog, fatigue, dizziness, and pain. I was told not to worry about additional MRIs—that they couldn’t be responsible for these symptoms. But could they be? —Casey
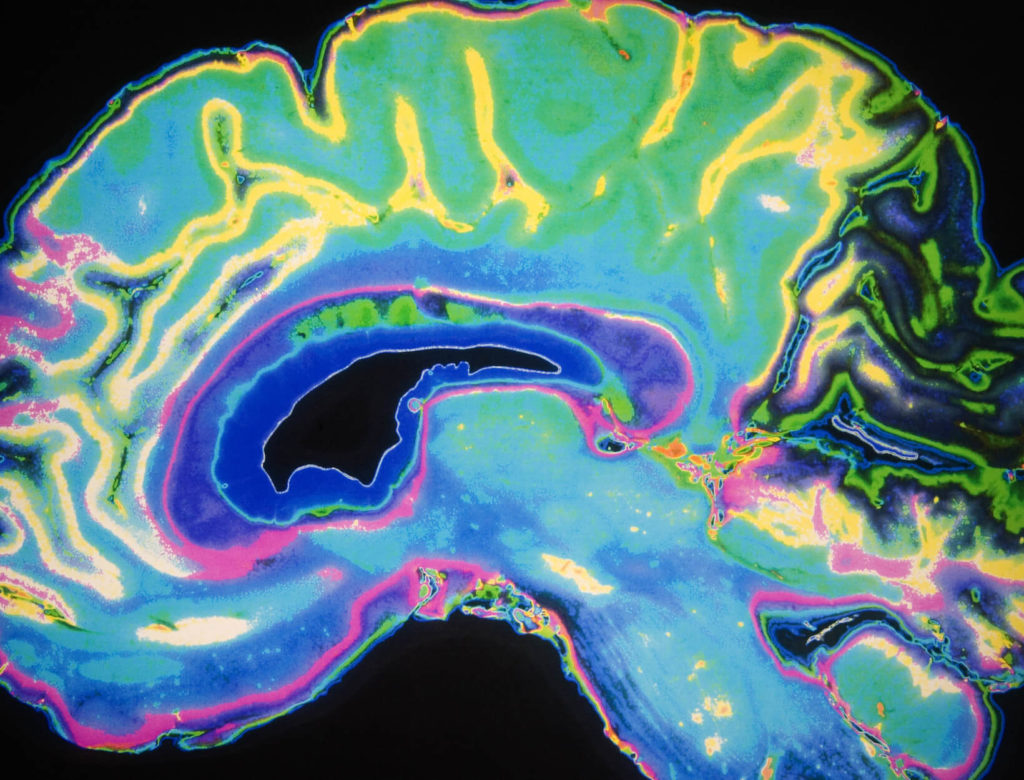
Hi, Casey. Yes, it is possible that an MRI (magnetic resonance imaging) dye could be responsible for these symptoms. (I hope your doctor has checked out other possible causes also.) An MRI is used to obtain an image of body tissues and organs. And for some MRIs, dyes—called contrast agents—are injected into the body to improve the visualization of tissues. Most of the dyes contain the heavy metal gadolinium, which appears to be a major culprit.
I’ve had a number of MRIs myself, and when researching the answer to your question, I realized that contrast agents were likely the cause of an unpleasant metallic taste in my mouth that lasted for a number of years. Given how common MRIs have become, it was disturbing to read about the myriad possible side effects of MRI dyes.
Allergic reactions—such as hives—to contrast agents are rare, but given that hundreds of millions of MRIs have been carried out worldwide, tens of thousands of people may have experienced reactions serious enough to lead to hospitalization. The possibility that you experienced an allergic reaction should not be dismissed.
And the problems with gadolinium are not limited to allergies. It was assumed that contrast dyes were harmless and quickly excreted but later discovered that gadolinium accumulates in the brain, bones, and organs. The amount of gadolinium deposited varies depending on the chemical makeup of the dye.
A group of physicians and researchers proposed the name gadolinium deposition disease (GDD) to describe persistent symptoms—including the ones you’ve described—arising after administration of gadolinium. Some of the symptoms their patients reported were brain fog, headache, bone and joint pain, and thickening of tissues under the skin.
In 2021, nine physicians self-reported symptoms of GDD, with the most common being brain fog, fatigue, muscle twitches, headache, insomnia, and burning, prickling, or tingling sensations in the legs, feet, and hands. The evidence is too preliminary to link these symptoms conclusively to gadolinium, but it warrants further consideration. Unfortunately, there’s very little evidence as to how to treat GDD. Some improvement in symptoms was reported in one study when chelating agents were used to remove gadolinium from the body, but this finding still needs to be validated.
The consequences of using gadolinium-based dyes are mostly unproven, but there is one that is widely accepted: Certain contrast agents containing gadolinium are tightly linked to a rare disease—nephrogenic systemic fibrosis—in people with kidney disease. Because of this, as of 2017, the European Medicines Agency has removed from the market the dyes that deposit the most gadolinium in tissues—Omniscan, Magnevist, and Optimark—and restricted the use of MultiHance. The FDA has not banned these dyes but recommends not using them in people with kidney disease.
In addition, the FDA recommends limiting the use of gadolinium-based dyes whenever possible. This is most important when you may need multiple MRIs, such as people with dense breasts who require MRIs for breast cancer screening. Whether alternatives to gadolinium-based dyes are a reasonable choice is something that people are determining together with their doctor, because the risks and benefits are highly individual.
MRI remains an essential tool for diagnosis and more. When I had unexplained vertigo and hearing loss, I felt lucky to have access to high-tech procedures like MRIs. The cause of my symptoms turned out to be a brain tumor called an acoustic neuroma which was successfully removed. Let’s use these procedures wisely, while realizing that many medical interventions have side effects.
MRIs don’t use radiation, which is a good thing. In MRIs the body is imaged using magnets. X-rays, CT scans, PET scans, and mammograms use radiation, and the American College of Radiology suggests that you keep track of the amount of radiation you are exposed to through medical imaging. We’ve summarized some things to know about these procedures in our goop PhD article on breast cancer. It’s important to be able to discuss diagnosis and treatment options with your doctor. And it’s important to work with medical professionals who listen to you.
This article is for informational purposes only. It is not, nor is it intended to be, a substitute for professional medical advice, diagnosis, or treatment and should never be relied upon for specific medical advice. To the extent that this article features the advice of physicians or medical practitioners, the views expressed are the views of the cited expert and do not necessarily represent the views of goop.

