Wastewater data from three counties in the Bay Area — San Francisco, San Mateo and Santa Clara — shows the concentration of coronavirus in the community has trended upward since April, and at some plants, levels rose as high as the January peak when the original omicron variant drove up cases.
Data from the first half of this week hints at a downward turn, but more data is needed to determine if the region has hit its peak, said Alexandria Boehm, a professor of engineering at Stanford who is part of team tracking California’s COVID-19 pandemic through wastewater analysis.
“It’s hard to discern true downturns from the short period variability,” Boehm said. “I think we need to see if we see sustained downturns over a week to call it a true downturn.”
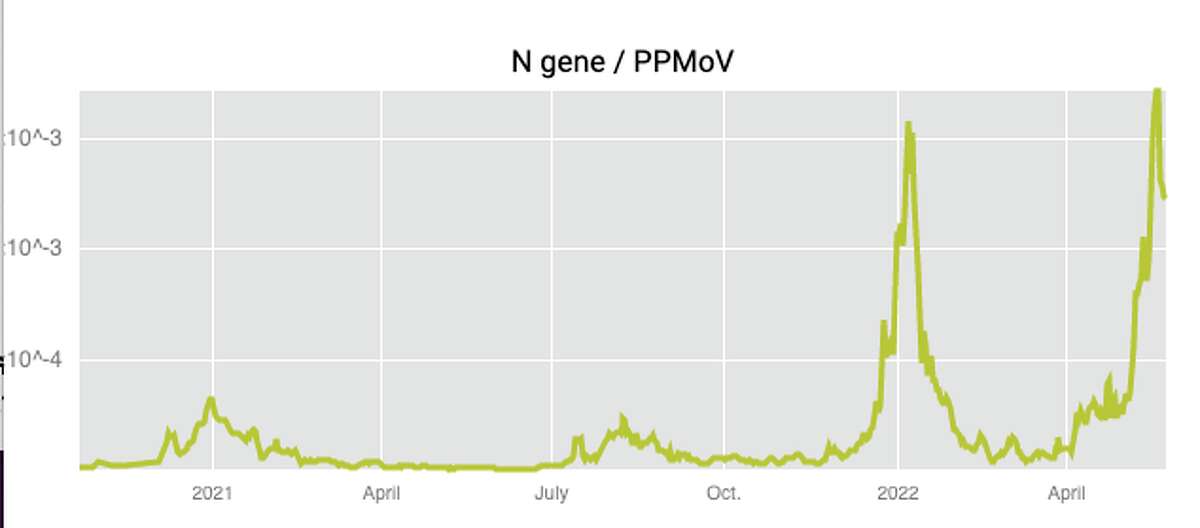
Wastewater data from the Oceanside sewage plant in San Francisco show that the levels appear to have turned down, but are still almost as high as during the omicron surge.
https://soe-wbe-pilot.wl.r.appspot.com/Wastewater data has been a helpful tool throughout the pandemic as infected individuals often begin to shed the virus before they test. The data can provide an early warning of surges and new variants, and also captures asymptomatic cases in people who may never test. More recently, it has become increasingly important as rapid antigen tests become widely available and people test at home.
“People aren’t reporting at-home tests to public health agencies so any data from government agencies right now is going to be vastly underreported,” said Boehm.
But while wastewater may offer a clear picture of the prevalence of the coronavirus in a community, it doesn’t capture the burden of disease. For this, you have to look at hospitalizations and deaths, and current figures indicate that the current situation is resulting in significantly less severe illness than in past surges.
“Since cases became ‘decoupled’ from hospitalizations in places with high vaccination rates with delta and omicron (like we have in the Bay Area), I suggest a hospitalization metric to determine the burden of disease in a community of COVID-19,” UCSF infectious diseases expert Dr. Monica Gandhi wrote in an email.
Current data shows a small increase in hospitalizations in San Francisco amid the recent surge in cases, but the increase is much less significant than in past surges. Also, Gandhi noted that when looking at hospital data, it’s important to keep in mind that many hospitalizations included in public health agency data includes incidental cases where someone went to the hospital for a surgery and happened to test positive for COVID-19. People with an incidental case are not in the hospital for serious COVID-19 illness.
Immunity from vaccinations and prior infection, boosters and variants that cause less severe illness are all reasons for the lower hospitalizations in this surge. (You can read more about hospitalizations in the SF Bay Area on SFGATE.)
BA.2.12 is the dominant variant in the San Francisco Bay Area
Wastewater data shows the highly contagious omicron subvariant BA.2.12.1 is the dominant strain. Cases of BA.4 and BA.5 are appearing, but not in abundance.
Boehm said her team is closely tracking BA.4 and BA.5 as a significant increase could suggest it’s overtaking BA.2.12.1. In South Africa, BA.4 and BA.5 became the dominant variants over BA.2.12.1, but Boehm said that as of now, there’s no indication that’s happening in the Bay Area.
“We’re measuring BA.4 every day now at all the plants,” she said. “We’re looking at whether we’re seeing a sustained increased and that would tell us whether it’s able to compete with BA.2.12.1. We’ll be able to tell that before the clinical data gives us that info.”
Research indicates that the first omicron variant causes less severe disease than past variants such as delta, and early studies show that the subvariants also lead to less severe illness. But the variants are highly transmissible.
“BA.2.12.1 is thought to be 25% more transmissible than BA.2, which is itself 30% to 80% more transmissible than BA.1, which is itself 200% more transmissible than delta,” UCSF infectious diseases expert Dr. Peter Chin-Hong said.