Over the last weekend of April 2024, something in Austin’s drug supply went horribly wrong.
The first deaths passed largely unnoticed by anyone other than the families and friends of those who consumed the tainted substances. An 8-year-old girl who’d been playing outside her apartment in northeast Travis County on the evening of Sunday, April 28, came home to find her 50-year-old father dead in bed. In a homeless encampment in a wooded area of East Austin, paramedics revived two people with naloxone, the overdose reversal drug known commonly as Narcan. But, hours later, one of them, a 51-year-old woman, was found dead inside her tent—a short walk from a 53-year-old man who likely died around the same time.
A clearer picture wouldn’t emerge, however, until 911 calls began flooding in the following morning.
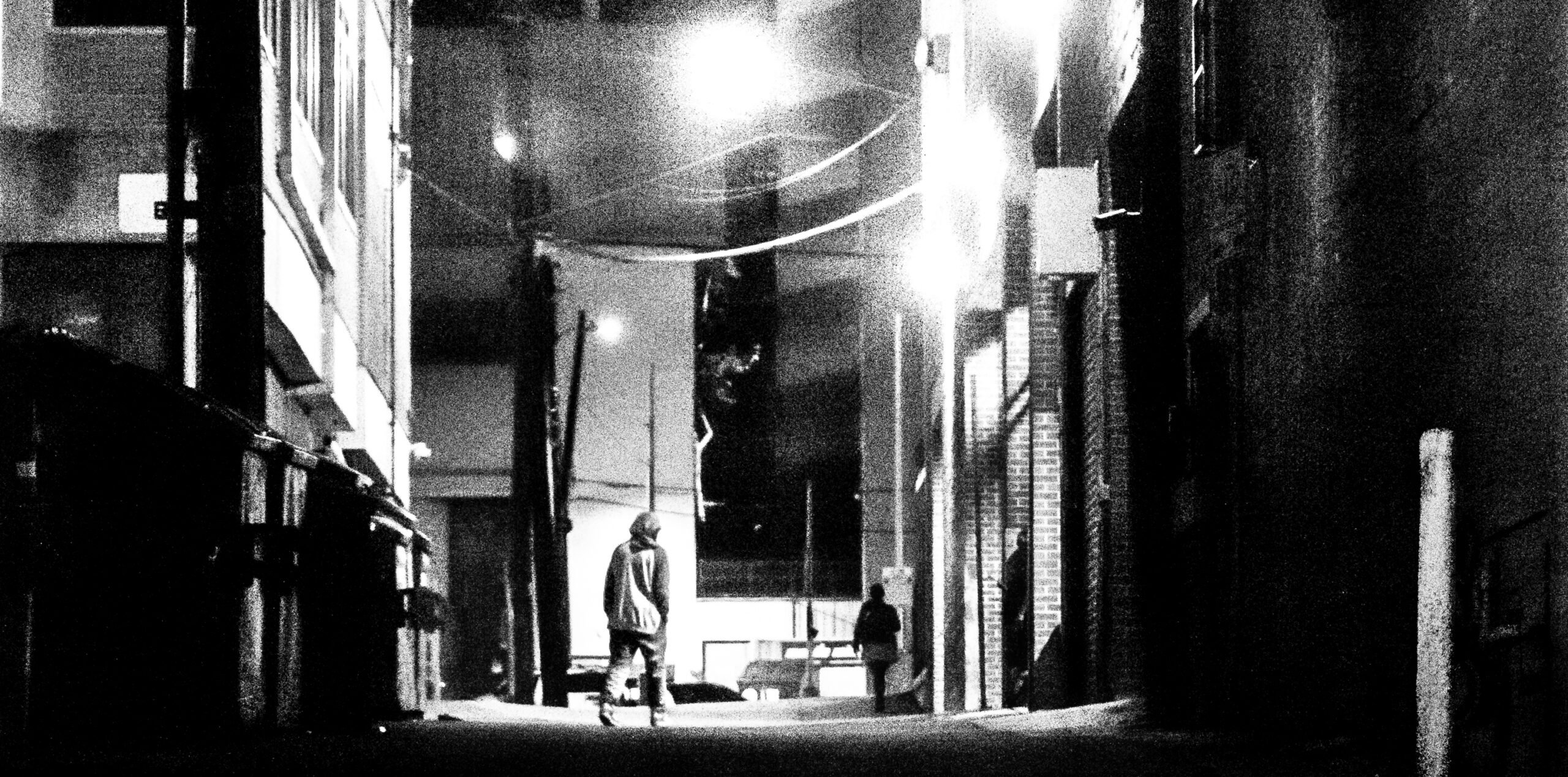
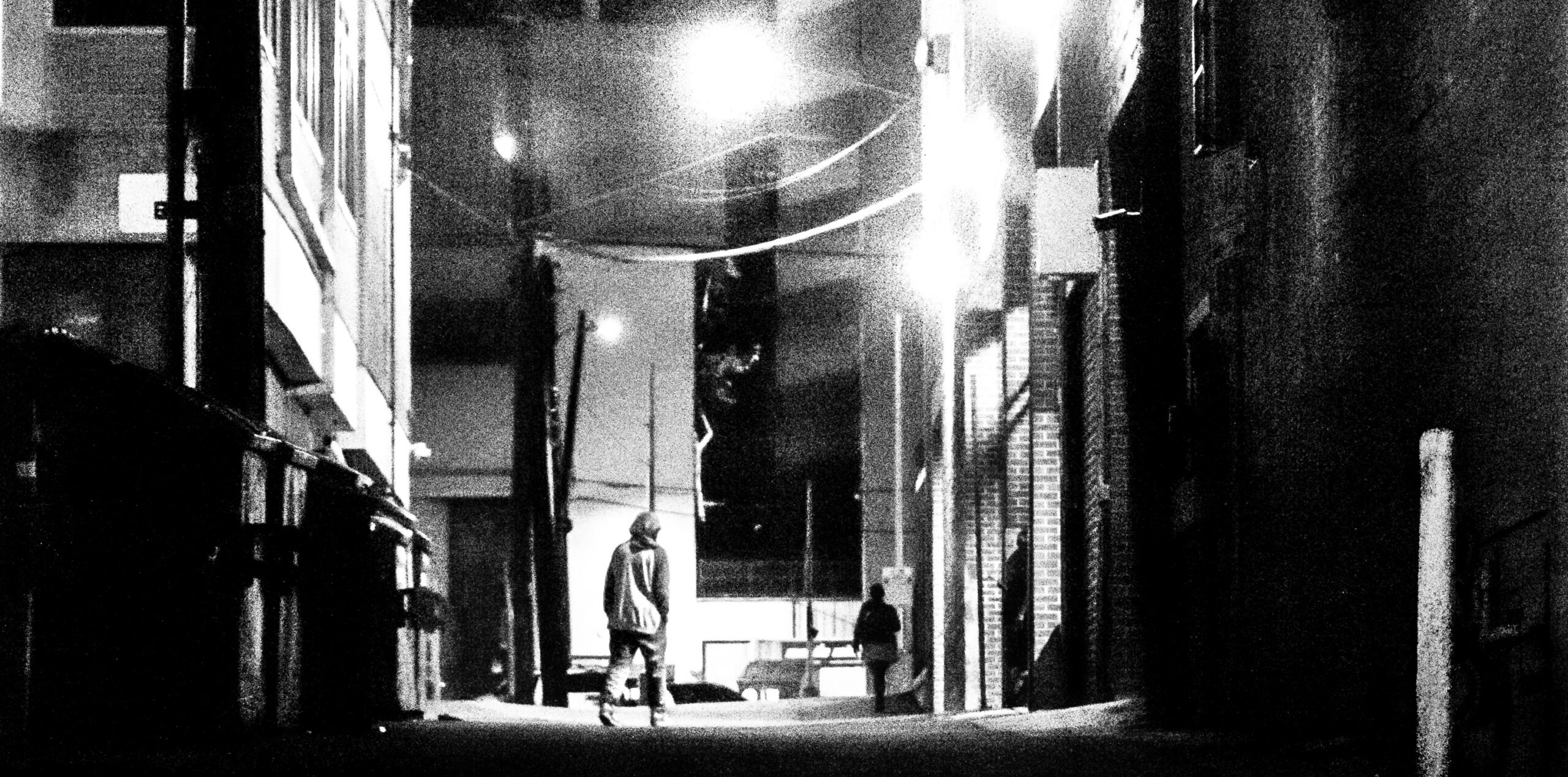
Most Mondays, the Sixth Street entertainment district would be quietly nursing the hangover from another rowdy weekend, the only souls on the street those who sleep in the shelters, alleys, and sidewalks. But emergency dispatchers were getting repeated reports of people in distress.
The first call came in just after 9 a.m. from someone calmly describing an overdose in an alley. But, as the minutes dragged on, panic crept into the caller’s voice. “I’m scared,” she blurted out. “Oh, my gosh, I’m so fucking scared. Somebody’s going to die because of these people.”
“What happened?” asked the operator.
“Somebody tried to say ‘Don’t call the ambulance,’” the caller responded. “Oh, my God. Oh, my God.”
A little before 10 a.m., a security guard flagged down one of the Austin police officers flooding the district. Two men were sitting on the ground next to a trash bin in an alley near Sixth and Red River Street, slumped forward. Only 20 minutes earlier, both men had been walking and chatting. Now, they weren’t breathing.
The officer administered naloxone and began performing CPR. Paramedics took one to a hospital. The other, 51-year-old Benjamin Arzo Gordon, couldn’t be revived.
The alley where Gordon died had become the epicenter of a mass casualty event. During a two-hour span that Monday morning, at least six others overdosed and were revived with naloxone in a four-block radius in downtown Austin. Over 72 hours, Austin police reported more than 70 overdose calls. Records from Travis County, which includes most of Austin, and neighboring Williamson County indicate that as many as 12 may have died. The culprit: a bad batch of crack cocaine.
“The closet is a very dangerous place for people who use drugs. It’s where stadiums full of people die every year.”
Through dozens of open records requests and interviews, the Texas Observer and Texas Community Health News have pieced together what happened during those deadly days—and how changes to state law might have saved lives. Across the capital city, people who consume crack, a stimulant, were suffering symptoms consistent with poisoning from opioids like heroin or fentanyl, the incredibly potent prescription painkiller.
The adulterated crack impacted Central Texans from many walks of life. Among the people who died were a construction worker from Honduras and a young man from Wimberley, who passed away in his parked truck with the engine running. Crack rocks found at the scene of some of the deaths tested positive for fentanyl.
A small, inexpensive item might have averted some of these deaths. Fentanyl testing strips can be used to check for the presence of the synthetic opioid. With an appearance similar to an at-home COVID-19 test, the strips are dipped in water in which a small amount of the drug has been dissolved. A line indicates if fentanyl is present.
But such testing strips are illegal in Texas. They’re considered paraphernalia, and possessing one is a Class C misdemeanor. While the Texas House passed a bill that would have legalized them in 2023, the Senate declined to vote on it.
In general, Texas has been reluctant to embrace the strategy of harm reduction, a broadly defined term for helping people who use drugs without stigmatizing or imposing strict parameters, while also involving drug users in planning and implementation. Harm reduction has been promoted in the United States since at least the 1980s. A classic early example is teaching people who inject drugs to clean needles with bleach, preventing the spread of HIV. The overall approach is sometimes pitched as a means to keep people alive long enough to get off drugs, but many practitioners simply seek to keep substance users safe and healthy, regardless of plans to enter treatment.
Under the administration of President Joe Biden, the federal government embraced aspects of harm reduction. Some states have as well. But policies favored by many Texas officials reflect the singular goal of making it as difficult as possible to use drugs. As it turns out, research and interviews with both experts and users of drugs show, making drug use more difficult also makes it more dangerous. Though Texas ranks low among states in fatal overdose rates, federal data shows the Lone Star State’s rate stayed nearly flat from 2023 to 2024, while overdose deaths fell significantly nationwide.

Among those calling for more humane drug policies in Texas and beyond is a coalition of academics, activists, service providers, and people who use drugs who argue criminalization endangers people with little benefit. Some members of this coalition identify as harm reductionists, while others identify as advocates for drug user health. Some argue that stigma and marginalization do more harm than drugs themselves; many believe that, while kicking drug habits should be the ultimate goal, the best tactic is to meet people where they are. These advocates push for more access to naloxone, legalized drug checking, and reduced stigma so that policymakers, service providers, and drug users and their families can have real conversations about how to stay alive.
In recent months, top Texas officials have not only rejected harm reduction but have also openly antagonized those who practice it.
The prevailing attitude in the state is, “Why should we try and save their lives? They’re just going to use again,” said Joy Rucker, a nationally known advocate who launched Texas’ largest harm reduction nonprofit. In California, where she used to work, harm reduction organizations get robust public funding and operate openly.
“Texas was just a rude awakening,” she said.
A tall, thin Houston native with a quick sense of humor, Benjamin Arzo Gordon had been living on the streets of Austin for years. A January 2024 photo in the Austin American-Statesman shows him with a close-cropped white beard and a gray beanie, at Central Presbyterian Church downtown, looking pensive as he discusses harsh winter weather.
Andi Brauer, who oversees the church’s homeless outreach programs, said Gordon was a regular at weekly free breakfasts, cracking jokes with her and other volunteers and taking a genuine interest in her wellbeing.
“He’d always say, ‘You need to sit down and eat,’” Brauer recalled. “Or, if somebody was sometimes threatening or rude to me, he would say, ‘Don’t mess with Andi.’” She once printed out a photo of the two of them and used it to make a card for him.
In the alley where he died, Gordon was known to stop by with meals from the nearby food truck where he worked. “He used to help people in the alley,” said Loretta, a 55-year-old Austinite who herself suffered an overdose after Gordon.
Bokhee Chun, a Central Presbyterian volunteer, remembered Gordon would sing her hymns. Some months before he passed, Brauer said, Gordon came in to fill out a volunteer application.
Like many who died last April, Gordon was an experienced drug user. His drug of choice, crack, put him at little risk of sudden death by itself. But the crack he smoked that spring day was laced with a substance that has become synonymous with America’s failed drug policies.
In the latter half of last century, as states and the federal government increased penalties for drug sale and use, overdose death rates stayed relatively flat. That raised questions about whether deterrence policies did anything to reduce drug use. Then, this century, overdose rates skyrocketed, driven by synthetic opioids including fentanyl. Fentanyl had been around for decades, but in the 2010s it increasingly caused deaths in northeastern states. As it moved west, the nation’s drug supply transformed.
Initially, fentanyl was used alone or to boost the potency of other opioids and depressants like heroin and prescription pain pills. But, in recent years, people killed by fentanyl are increasingly found to have stimulants like cocaine or methamphetamine in their systems. Explanations for this vary. Stimulants may be intentionally adulterated to hook users on fentanyl. A stimulant user might take opioids to come down. An unsophisticated dealer with a small stimulant supply may add fentanyl to stretch it. And failure to clean scales or surfaces can also mix fentanyl with another drug.
In Texas, overdose rates increased dramatically starting in 2020. From June 2023 to June 2024, more than 5,000 people died of an overdose in the state, with Travis County recording the highest fentanyl-related death rate among Texas’ most populous counties in recent years. Though Texas has one of the lower overdose rates in the nation, deaths in the state declined by less than 3 percent from 2023 to 2024, while the rest of the nation saw a drop of nearly 15 percent, per the federal Centers for Disease Control and Prevention. In October, the Texas Department of Health and Human Services (HHS) announced that it recorded a 13-percent drop in the state over the same period—but its figures include only those overdoses deemed accidental, not those labeled intentional, suicide, or of undetermined cause.
Experts also question the general accuracy of Texas’ numbers. In much of the state, underfunded and under-trained justices of the peace are charged with death investigations. Overdoses, which require costly autopsies and toxicology reports, are easy to overlook.
In response to the overdose increase, HHS in 2017 launched the Texas Targeted Opioid Response (TTOR) initiative. HHS is also part of a state awareness campaign using billboards and social media ads focused on cautionary tales of young Texans who overdosed. At the same time, state leaders have doubled down on criminalization.
In 2023, the Legislature passed a law allowing prosecutors to bring murder charges in fentanyl overdose cases. Critics say this discourages people from reporting emergencies, and research shows such laws harm public health. Some who overdosed in Austin last April had shared drugs, putting survivors at risk of being charged. In 2021, the Legislature passed a good samaritan law ostensibly meant to protect people who call 911 to report an overdose. The law created a defense for people arrested for low-level possession, but it has so many caveats—you can only use it once in your life, it doesn’t apply if you’ve been convicted of a drug-related felony, you can’t use it if you’ve reported another overdose in the last 18 months—that you’d need a flow chart to understand it. Critics say the statute’s of little use.
“The fentanyl-induced or the drug-induced homicide laws, that jacks up the consequences and the intensity so much more,” said Alex White, director of services at the Texas Harm Reduction Alliance, an Austin nonprofit that does street outreach, operates a drop-in center, and provides supplies including for hygiene and wound care.
Some states, like Maryland and Vermont, make a point of prioritizing input from people who use or have used drugs while crafting policy. Harm reduction advocates say this is lacking in Texas, though HHS does have a low-profile advisory committee that is required to include members who’ve received mental health or addiction treatment.
“If you’re thinking that you know how to serve folks, and you don’t have those folks at the table when you’re trying to serve them, it’s not going to work,” said Stephen Murray, a paramedic and overdose survivor on Massachusetts’ Harm Reduction Advisory Council.
Rapid changes in the drug supply can make it difficult to conclusively track policy impacts. Critics blame Texas’ persistent overdose rate at least partly on punitive laws, but a few western states including liberal Oregon—which famously passed a drug decriminalization ballot measure in 2020—actually saw overdoses increase between 2023 and 2024. To this, some experts and at least one study counter that fentanyl’s delayed arrival on the West Coast has distorted the death rates, and that Oregon specifically did not implement sufficient services alongside decriminalization.
Texas Governor Greg Abbott’s office did not respond to a request for comment for this story.
Loretta woke up on the morning of Monday, April 29, in the alley where she often goes to smoke crack and sometimes spends the night. She grew up in East Austin, only blocks away.
Loretta said she lent her pipe that morning to a friend who’d just purchased drugs. Then she heard someone ask, “What’s wrong?” and saw the friend staring up, trance-like.
“He stayed looking at the sky,” Loretta said, reclining and rolling back her eyes to demonstrate. “The next thing I know he just went like this,” she said, as she pantomimed slumping limply to the side. “I was shaking him, and I said, ‘What’s wrong, what’s wrong?’ And after that he just didn’t answer.”
Despite fear she’d be held responsible, Loretta yelled to a friend to call 911. Police and paramedics swarmed the area. Loretta watched as someone else collapsed. “She hurt herself hard on the concrete and I said, ‘Oh, my God, hell no, this is not happening.’”
Soon, an acquaintance ran up to say Loretta’s boyfriend had also collapsed in a nearby portable toilet. “He was slurring like a baby, like a little boy,” Loretta said. “He started to lose consciousness. I slapped him hard. It hurt my hand. And I shook him and I started praying.”
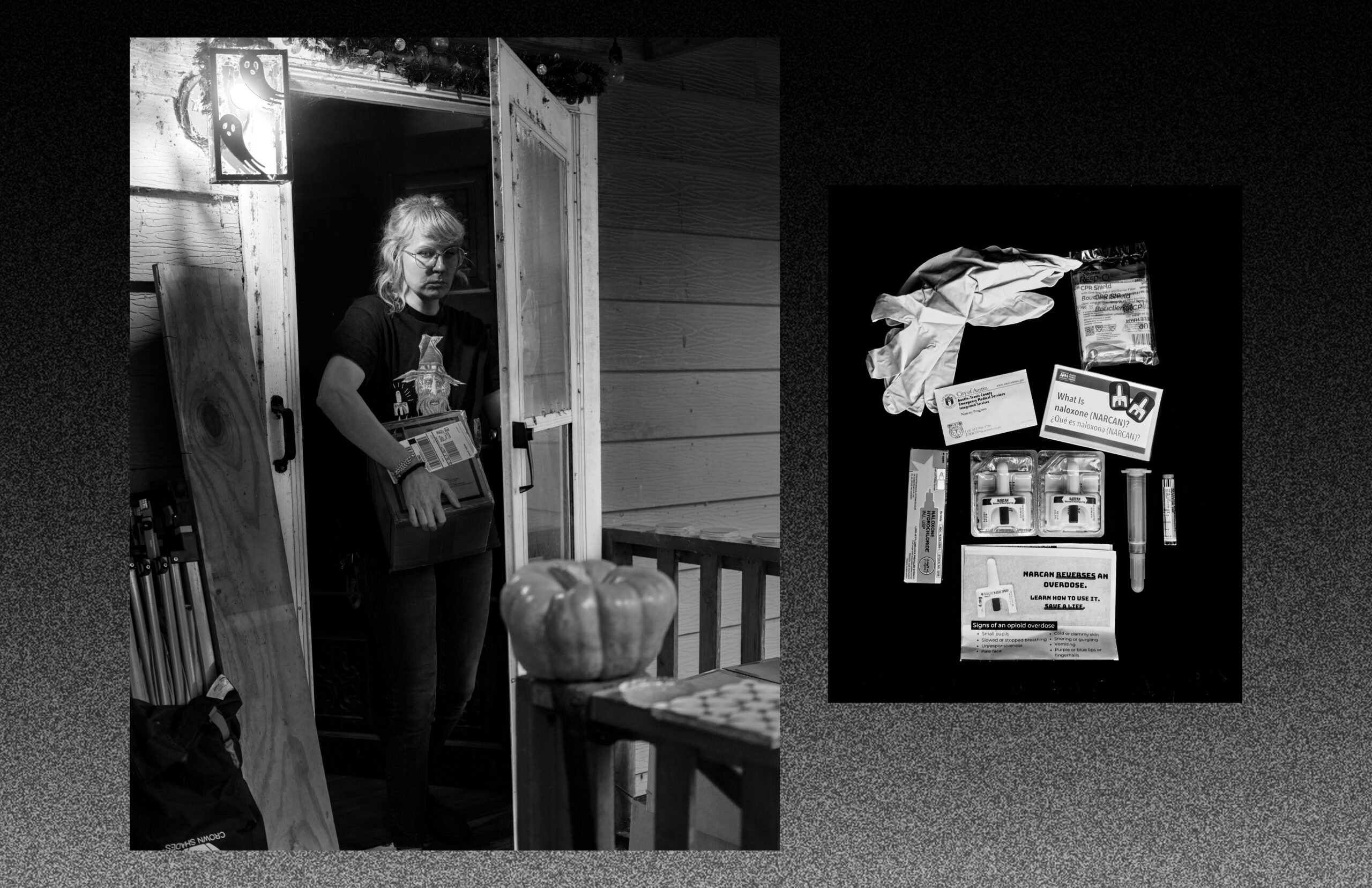
Around the time that Loretta was calling out for help for her boyfriend, and EMTs were trying unsuccessfully to save Gordon, Adam Balboa showed up to work at an Austin-Travis County EMS (ATCEMS) station in south Austin. A case manager for a unit focused on substance use, Balboa heard the overdose reports and symptoms being described and knew what would save the most lives. “We needed to flood the downtown area with as much Narcan as possible,” he said.
Opioids in the bloodstream bind to receptors in the brain, creating euphoria. But by a quirk of physiology, excessive opioids bound to those receptors interfere with the body’s ability to measure its need for oxygen, slowing breathing—to the point where it can be fatal. Mouth-to-mouth resuscitation can keep someone alive. Narcan temporarily blocks the receptors to opioids, essentially short-circuiting an overdose if delivered in time.
The medics and police officers in downtown Austin were running out of naloxone, but Balboa didn’t just want to get them more. He also wanted to get it in the hands of people who use drugs, along with their friends, family, and neighbors. So he and colleagues began throwing together kits containing Narcan, a CPR mask, and instructions, and he hurried downtown with his SUV loaded up with the blue zippered pouches. “Everybody was super receptive,” he said. “They were clipping it to their belts and … going about their normal business.”
As common-sense as that response seems, it’s one strongly associated with harm reduction. By handing out naloxone downtown, Balboa was helping those most vulnerable to the tainted drugs help one another. It’s also a response that would have been impossible a few years ago.
“I’m telling the kid that came to get me specifically … ‘Because of you, this woman is alive.’”
Balboa’s unit is the brainchild of Mike Sasser, a 51-year-old ATCEMS captain who’s been in recovery for 21 years. A longtime paramedic who often worked with Austin’s unhoused population, Sasser became friends in 2018 with Mark Kinzly, a lion of the Texas harm reduction movement. Kinzly, who passed away in 2022, had helped start the Texas Overdose Naloxone Initiative, which was getting grants to distribute the medication. He had a seemingly simple idea for Sasser: ATCEMS could use grant money to buy Narcan, pass it out, and train people how to use it.
“My mind was blown,” Sasser said. “Why have I never thought about this? That would save so many lives.”
ATCEMS doctors then wrote prescriptions that allowed medics to hand out naloxone (today, it’s available over the counter). Sasser’s unit also began reaching out directly to overdose survivors and administering a maintenance drug that reduces opioid cravings, and it now includes two full-time case managers who run an overdose reversal education program called Breathe Now.
All of this fits under the philosophy of harm reduction, which can also include teaching people to use drugs more safely and providing supplies like clean glass pipes, which help prevent disease and infection. Providing food, water, hygiene products, or wound care to people who feel stigmatized in doctor’s offices is another tenet.
“We want to provide people with what they need, so we can build that trust,” said Em Gray, whose NICE Project provides supplies to Austinites, many of them unhoused, and stocks Narcan vending machines. “That’s how we show that we are there for them; we’re there to improve their quality of life, there to reduce their overdose death rates.”
There’s little funding available in Texas for the nonprofits and mutual aid groups that do this work. Across the state, harm reductionists often operate out of backpacks or car trunks.
To the state’s credit, Texas has taken some steps to increase naloxone distribution. TTOR does this with an annual federal grant of about $5.5 million. In 2019, TTOR, whose Narcan distribution program is administered by the University of Texas Health Science Center at San Antonio, gave about 40 percent of its naloxone to law enforcement agencies—even as research shows it’s more effective to give the medication to laypeople, who are typically first on the scene and present no threat of arrest—an analysis by Texas Community Health News found. By 2022, TTOR’s emphasis had shifted, with law enforcement making up only about 15 percent of its distribution.
But police are still prioritized in Texas’ long-term naloxone plan. Under a different state program started in April 2023, the Texas Department of Emergency Management (TDEM) began distributing $75 million worth of the medication over 10 years. That naloxone, donated by a pharmaceutical company as part of a court settlement over opioid deaths, is largely earmarked for first responders. Of the more than 150,000 doses that TDEM distributed from April 2023 to September 2024, 118,000 went to law enforcement agencies, mostly sheriff’s offices. Many of these offices cover areas that lack other harm reduction infrastructure, but records provided by TDEM show sheriffs aren’t using the naloxone. Of 13 counties in which agencies reported using doses from TDEM by September, the highest rate of use was 3 percent. Much of that naloxone will expire later this year. In an email, a TDEM spokesperson said the agency had “yet to turn down a request for naloxone” and that “Administration or disposition of distributed naloxone is up to the receiving entity how they see fit, in accordance with manufacturer’s guidance.”
When it set the state’s two-year budget in 2023, the Legislature allocated an additional $18 million in opioid settlement funds to UT Health San Antonio, but it’s not clear the appropriation will be renewed.
In the meantime, harm reductionists rely on a patchwork of naloxone sources, including local governments.
“Had we not saturated Austin with Narcan leading up to [the April] event, then that event would have been a lot more detrimental than it was,” said Sarah Cheatham, a peer support specialist with The Other Ones Foundation, an Austin nonprofit serving the unhoused. “Even when it was hard to get in our hands, we were out there doing this communication for months before this happened.”
By late morning on April 29, the Austin Police Department (APD) had some idea what was happening. Crack rocks and pipes had been found at the scene of a number of overdoses in an area known for its use, and officers had interviewed some who’d been revived with naloxone. They began looking for people seen on surveillance cameras and suspected of selling the tainted crack. While responding to an overdose, detectives found one suspect standing in front of a tent, just a block from police headquarters.
While cops made arrests, harm reductionists tried frantically to figure out what was going on. A little after noon that Monday, Claire Zagorski, a graduate research assistant at the University of Texas at Austin who’s worked in harm reduction for years, messaged a group chat: “Austin folks there’s a bad batch downtown as of this AM. Not sure on specifics but it does respond to naloxone.”
Groups started handing out Narcan and warning the communities they serve, but without any official information from local governments. “We were really just kind of going in blind,” Cheatham said. “We were all talking to each other about, ‘Who’s going to these camps? Where is it happening? Is it happening downtown?’ And I was mainly reaching out to the people that I know.”
Research shows that, given the chance, drug users will reduce their risk of overdose—including by carrying naloxone, not using alone, or taking a small tester dose. But, lacking detailed information, harm reduction workers in Austin were constrained. “It’s distressing that the thing that got everyone activated was me being notified by a backchannel,” Zagorski said.
When local officials finally made public statements hours after the flood of 911 calls, they only addressed some questions. Whatever was killing people was responding to Narcan, officials said, in a news release and press conference. But they were vague about which drug was adulterated, and there was no mention of test strips.
“It was a very chaotic scene at first,” APD Lieutenant Patrick Eastlick told the Observer. “Something we can look at in the future is, if this happens again, that we reach out to these different groups where we can spread the word.”
Open conversations about drugs are difficult in a state where top elected officials are cracking down on services for people who use them. In late November, state Attorney General Ken Paxton filed a headline-grabbing lawsuit to shut down a homeless navigation center at a south Austin church. The suit specifically blames the Texas Harm Reduction Alliance’s needle exchange program for “the prevalence of drug paraphernalia, including used needles, littering the surrounding area.” Drug use around the church “fuels criminality, and creates an environment where nearby homes and businesses are at constant risk of theft,” the complaint states.
Critics say efforts like Paxton’s just push drug use out of sight, creating greater risk. “It sends the message to people who use drugs that they should hide it, they should be kept in the dark and in the closet,” said Aaron Ferguson of the Texas Drug User Health Union. “The closet is a very dangerous place for people who use drugs. It’s where overdoses happen. It’s where stadiums full of people die every year.”
At least two who died in the Austin overdose outbreak were found alone. Family members of at least two others who perished at home told police they didn’t know their loved one had used drugs that day.
How state officials talk about drug use, critics note, also suggests that only some lives matter. For example, in a 2023 legislative hearing, GOP state Senator Drew Springer—in a successful attempt to woo conservative support for requiring school districts to stock naloxone in middle and high schools—distinguished between different groups of Texas children. “I think the general public, when they hear ‘overdosing,’ they think ‘That’s just a druggie, and that’s a druggie kid’s problem,’” he said. “No, it’s your kid’s [problem], because he may be taking a Xanax or an Adderall” without knowing fentanyl was present.
Claudia Dambra, who runs Street Value, a drug user health organization in Houston, criticized messaging that condemns certain substance users. “All it’s doing is creating more separation,” she said. “It feels like this weird, forced social Darwinism. … It feels like they’re picking us off.”
In an email, an HHS spokesperson said the agency does not discriminate: “[HHS] substance use programs offer treatment and recovery support for people, regardless of substance use duration.”
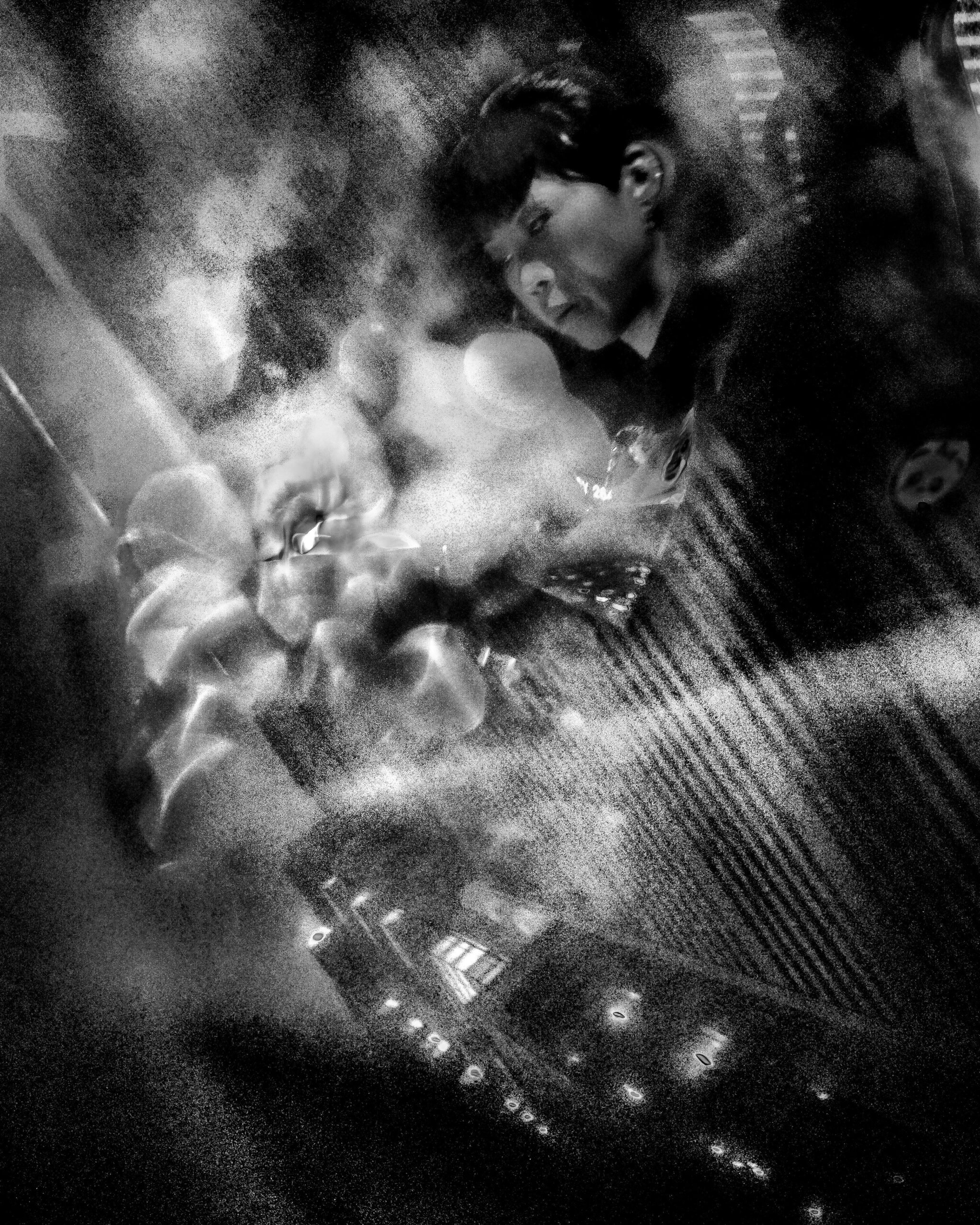
After the horror of watching her boyfriend taken away in an ambulance, Loretta wandered through downtown Austin. Near APD HQ, in the area where police had arrested their suspect earlier, she was offered crack that her friend insisted came from a reliable source. Stressed and scared, she took a hit.
“I started getting a headache right away, like oh, my God, I’ve got a migraine or something. And I started throwing up,” she said. “I said, ‘Call the police, I’m sick.’”
Loretta didn’t lose consciousness, but she was vomiting as police questioned her. Eventually, she was taken to a hospital. She would be among the survivors.
Today, Loretta says that she gets test strips from harm reduction organizations, which quietly distribute them despite state law, and she gives them to friends. But, at the time, she knew little about them. Organizations that distribute strips generally can’t use grant money for their purchase, and government agencies, like ATCEMS, don’t distribute them.
Back in 2023, it seemed Texas was poised to legalize the strips. Before that year’s legislative session, Abbott said he supported allowing the tests, and legislators in both chambers introduced bills to legalize equipment for checking a range of drugs. One by Houston-area Republican Tom Oliverson, which was limited to fentanyl strips only, sailed through the House.
Oliverson, an anesthesiologist who has prescribed fentanyl to patients, said he’d heard from family members of people who purchased black-market pills without knowing they included the powerful opioid.
“That’s literally like stepping on a landmine,” Oliverson told the Observer. “You heard a click and the next thing you know, you were gone. Nothing you could have done could have saved you. You didn’t know it was there, right? Except for the fact that there are test strips.”

The bill received tepid support from harm reductionists, who were frustrated by its narrowness. The drug supply is constantly changing: Today, the dangerous veterinary tranquilizer xylazine is increasingly used to supplement other drugs. “We’re really trying to craft language that’s inclusive,” said Cate Graziani, former head of the Texas Harm Reduction Alliance and current co-director of a spinoff advocacy group, Vocal TX. “We don’t want to go back to the Legislature every time we have a new overdose prevention tool.”
Oliverson said the bill only applied to fentanyl “because it is that much more dangerous, because it is that much more powerful. … People say to me, ‘I don’t like the idea of giving people test strips because it gives them confidence in the illegal drugs that they’re buying, and I want to discourage people from using illegal drugs,’” he said. “Well, I want to discourage people from using illegal drugs too, but having them insta-killed by a mislabeled pill that they bought, the first time they took it, is not an effective strategy for recovery.”
While other drug-checking legislation failed that session, Oliverson’s bill passed the House 143-2—but it never received a hearing in the Senate Criminal Justice Committee. “They just could not get over the idea that you are making it safer for people to use illegal drugs and that we shouldn’t make it safe for people to use illegal drugs,” Oliverson said, “because they shouldn’t be using illegal drugs at all.”
Oliverson said he’ll introduce a similar bill this session and may rewrite it to include xylazine, but he made it clear he doesn’t support other harm reduction measures like needle exchanges. Such a bill will simply fizzle again, though, barring a change of heart in the Senate, which is run with an iron fist by Republican Lieutenant Governor Dan Patrick, whose office did not respond to arequest for comment for this article.
“It’s so demoralizing to live in a state where your elected leadership is so unwilling to do something so small as legalizing fentanyl test strips, because there’s so much stigma around drug users,” Graziani said.
By the afternoon of April 29, the tainted crack had made its way to south Austin. Loretta Mooney, another ATCEMS case manager in the substance use unit, was off work but rushed in. Dispatchers could see a new cluster of calls developing on Oltorf Street, east of Interstate 35.
By the time Mooney responded to her first call, at an apartment complex, medics had administered naloxone and revived a woman. Mooney handed out a few doses, then responded to another call from a fast food restaurant across the street. Someone had flagged down police, concerned about a man collapsed against the restaurant’s wall. Officers began CPR and administered Narcan. Mooney gave the man an additional dose and continued life-saving measures. Still, the 53-year-old died.
The situation was starting to look similar to downtown earlier in the day. Teenagers at another apartment complex began waving down Mooney and the officer. They ran over. Mooney administered naloxone to an unconscious woman and helped the officer deploy a breathing bag and mask. After a few minutes, the woman began breathing on her own again.
With Balboa now on his way to meet her and most of the calls near her covered, Mooney came to the same conclusion Balboa had that morning. “I was like, ‘Bring me all the Narcan you have and we’re going to start teaching these kids,’” she said.
On the lower level of a terraced parking lot, Mooney and the officer spread out naloxone kits and gathered the teenagers who had flagged them down.
“I’m telling the kid that came to get me specifically … ‘Because of you, this woman is alive,’” Mooney said. “We’re on the side of [the road] with, you know, ages 10 to 16, teaching them how to use Narcan.”
While Mooney and then Balboa, too, instructed people in the neighborhood how to use naloxone, a new crisis emerged. Some of the people who had bought the tainted crack were now behind the wheel. First responders were rushing to car wrecks and stalled vehicles.
Responding to the new calls, Mooney and Balboa saw the results of their impromptu training. As Balboa headed to a pawn shop where someone was overdosing, he got stopped in traffic. With his lights and sirens going, trying to weave through vehicles, he saw the teenagers they’d trained earlier.
“Before I can clear an intersection, they’d already sprinted over, pulled out a kit, and started giving Narcan,” he said. “Not only were they excited and ready to help and empowered to be able to do so, but when that opportunity finally came for them, they ran at it.”
As evening fell, the dying slowed. Behind closed doors, away from passersby armed with naloxone, however, it wasn’t through yet. A woman staying at a motel on Oltorf woke up during the night and called her 61-year-old husband, only to hear his phone ringing in the bathroom, then find him lying on the floor. The partner of a 57-year-old man got out of bed to get him warm milk after she noticed his nose bleeding, but, when she came back, he wasn’t breathing. A 36-year-old parked his truck in a lot in north Austin; when a security guard called 911 hours later, he was already dead. Around midnight, a son found his 63-year-old father deceased in an Oltorf apartment.
Later that same Tuesday, Loretta was released from the hospital. Downtown again, she found out her boyfriend had also survived and been released.
The following day, a man in southeast Austin woke up in the afternoon to find that a friend he’d let stay in his apartment had died while he slept. After agonizing for nearly two hours, he called the cops. That afternoon, a 34-year-old resident of Williamson County, just north of Austin, was found on the floor of his bedroom, where police found crack laced with fentanyl. Between April 28 and May 6, nine people in Travis County died from the toxic effects of fentanyl and cocaine, according to Travis County Medical Examiner records, in addition to the Williamson County death. At the request of APD, the Travis medical examiner withheld the cause of death in two other fatal overdoses that may have been related.
In the aftermath, APD made a handful of arrests. In some cases, police affidavits show, detectives were following information about who may have sold the tainted crack; in others, undercover officers simply went to known drug markets and arrested anyone who would sell to them. Eastlick, the APD lieutenant, said investigators believe the crack was adulterated at the local level, not higher up the drug supply chain, but that police had been unable to prove anyone intentionally sold tainted drugs. “It was a short surge … so our thinking is that it was not intentional,” he said.
As the tainted substance faded from the Austin drug supply, Cheatham said she and others heard stories of people who overdosed and were revived by naloxone without the authorities ever being alerted. In Austin’s camps and alleys, anonymous drug users helped one another.
Many of those who died remained anonymous as well, victims of an event whose details remained unclear and which took its toll mostly on the sort of people society tends to lose in its cracks.
Brauer and Chun, with the Central Presbyterian church, didn’t learn of Benjamin Arzo Gordon’s death until months afterward, when contacted for this story. In early November, the pair traveled to the indigent burial cemetery in northeast Travis County. In the wide, level graveyard, rows of nondescript markers rested flush to the ground. By Gordon’s, they left a bouquet of artificial flowers and a potted plastic plant.
“Just being able to picture him so clearly, knowing him as somebody that I value, that I enjoyed seeing, that was full of life and laughter despite the situation he was in—to hear about the way that he died of a drug overdose, probably fairly anonymously, just was incredibly sad to me,” Brauer said. “So because I didn’t get a chance to say goodbye … it just felt like something we needed to do to honor him.”
Editor’s Note: This article was produced in collaboration with Texas Community Health News and Public Health Watch. Daniel Carter contributed reporting.