HealthOne and UnitedHealthcare reached a last-minute deal to keep the hospitals in-network, averting a separation that would have forced patients to find new doctors or pay more out-of-pocket.
When patients visit a hospital that has agreed to in-network rates, they pay either a flat fee or a portion of the cost of their care. If they go to an out-of-network facility, they could get a bill for whatever their insurance declined to cover. Federal and state law prevent surprise bills when a patient has an emergency, but not for scheduled care.
The two parties reached a multi-year deal that ensures continued, uninterrupted network access to the health system’s hospitals, facilities and physicians for people enrolled in employer-sponsored commercial plans, individual family plans and Medicare Advantage plans, including group retiree and dual special needs plans, Cole Manbeck, a United spokesman, wrote in a news release to announce the deal.
“We thank our members and customers for their support and patience throughout this process. We are honored to continue supporting all of the people throughout Colorado who depend on us for access to quality and affordable health care,” the news release stated.
The two businesses existing contract ended Sunday, and the two sides struggled to agree on rates for the next contract. If they hadn’t reached a deal, patients covered by United would have paid more to use:
• Centennial Hospital
• North Suburban Medical Center
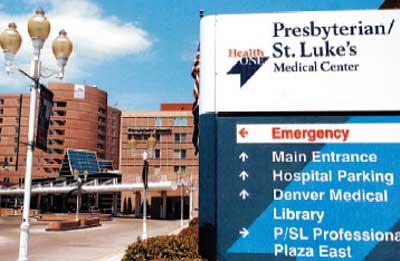
• Presbyterian/St. Luke’s Medical Center
• Rocky Mountain Hospital for Children
• Rose Medical Center
• Sky Ridge Medical Center
• Swedish Medical Center
• The Medical Center of Aurora
United accused HealthOne of making “unreasonable” demands for double-digit increases in rates, while HealthOne said United offered rates below market levels for the Denver area.
Health systems and insurers usually reach a deal before their contracts expire, but CommonSpirit Health left Anthem BlueCross BlueShield of Colorado’s network for more than two weeks earlier this year when they couldn’t agree on rates by the deadline.
At least 20 hospitals or systems had disputes with insurance companies nationwide in the second quarter of 2024, compared to at least 24 during the same period of 2023, according to Becker’s Healthcare Review. The true number could be higher, because the count relies on news reports, and some disputes could have ended quietly or happened in places without local media.
About 30% of the parties didn’t reach an agreement before their contracts expired, meaning the hospitals went out of network at least briefly, according to Becker’s, which is a trade publication.
United is the largest insurance company nationwide in the commercial and Medicare Advantage markets, while Tennessee-based HCA Healthcare, which owns the HealthOne hospitals, is the largest for-profit health system in the country.
Reporter Noelle Phillips contributed to this report.
Originally Published: