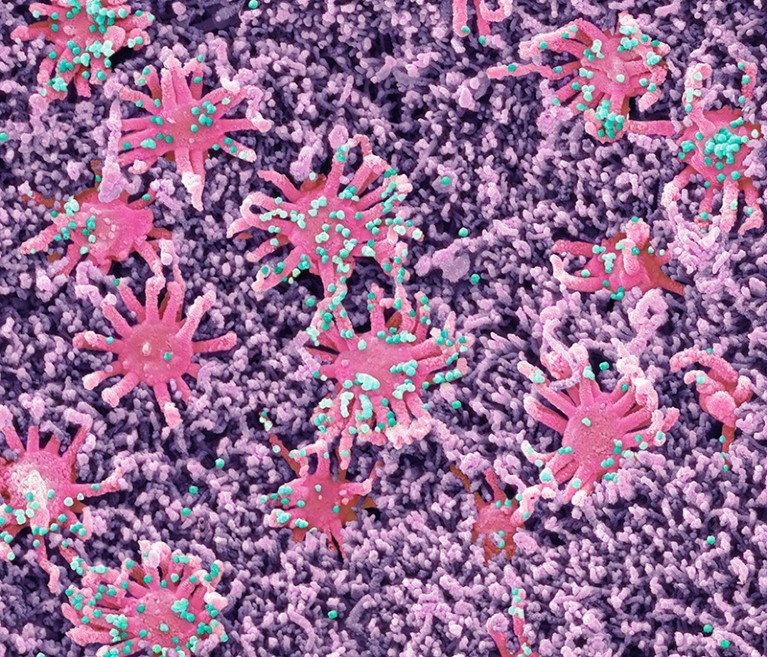
Particles (green) of SARS-CoV-2 are attached to olfactory cells in the nose.Credit: Steve Gschmeissner/Science Photo Library
During the throes of the COVID-19 pandemic, Anne Moscona didn’t feel safe going to a restaurant or catching a flight. And she wished she could feel confident that she could see her immunocompromised relatives without inadvertently spreading the novel coronavirus to them. All this made her work personal: for the last decade, Moscona, a molecular virologist, had been hunting for compounds that could stop viruses in their tracks, before the pathogens infect even a single cell in a person’s body.
Now Moscona, at Columbia University in New York City, and her colleagues have homed in on a compound that might foil SARS-CoV-2. Even better, it’s simply sprayed up the nose — no needle required1.
The spritz developed by Moscona’s team is one of a raft of proposed nasal sprays to prevent SARS-CoV-2 infection. The sprays would be fast-acting and would be applied frequently, perhaps once or twice a day, to the site where the virus first takes hold — the nasal lining and throat. Unlike vaccines, which train the recipient’s immune system to build long-lasting protection, the sprays are short-lived compounds that would directly block the virus’s ability to enter cells. Multiple research teams have shown that such sprays are effective at warding off SARS-CoV-2 infection in animals.
Fourth dose of COVID vaccine offers only slight boost against Omicron infection
If effective in humans, these compounds would be a welcome addition to the limited arsenal that researchers have developed against the virus, says Donna Farber, an immunologist at Columbia University in New York City. Vaccines protect against severe COVID-19, but they’re less adept at preventing infection, and current antivirals treat infection rather than preventing it. The sprays could offer people another way to avoid infection on top of — or instead of — wearing a face mask, especially in high-risk settings such as hospitals and restaurants. “They’re definitely worth pursuing in a big way,” she says.
Despite their promise, these sprays have a long way to go: Funding and interest from pharmaceutical firms for human trials has been limited, in part because trials to determine efficacy for prophylactics are large and expensive, says Moscona. And the sprays must achieve the difficult task of coating any surface to which a virus might attach, because once a viral particles enter even a few cells, a full-scale infection can progress rapidly.
Viral blockade
The effort to develop prophylactic treatments against viruses long predates COVID-19, says Wendy Barclay, a virologist at Imperial College London. Such research has paid off with a range of medications taken by mouth, including oseltamivir (Tamiflu), which protects against influenza infection, and tenofovir–emtricitabine, which prevents HIV infection. But, Barclay says, there are no prophylactic nasal sprays except First Defence, which is designed to act as a physical barrier against common-cold virus particles.
Prophylactic sprays have a simpler job than conventional antivirals, such as Paxlovid, that are used in the first days of an infection: preventing a single virus particle from infecting a cell is a “much easier ask than counteracting the effects of millions of viral particles” days after infection, Barclay says.
Researchers have been testing many types of compounds in nasal sprays to thwart SARS-CoV-2 infection. Among them are small antibody-like molecules called nanobodies, which disarm the virus by nestling into the nooks and crannies of viral proteins; short chains of amino acids called peptides; and small molecules that mimic proteins.
Why scientists are racing to develop more COVID antivirals
The prophylactic developed by Moscona and her colleagues, for example, is a peptide that gums up the virus’s machinery for fusing with a host cell. This prevents the virus from delivering its genetic payload into the cell, thus blocking infection.
To test their peptide, Moscona and her colleagues administered it into the noses of ferrets once daily for two days and co-housed the treated animals with another ferret that was infected with SARS-CoV-2. None of the six ferrets that received the peptide became infected with the virus, while all six ferrets that received a placebo dose did1. Before testing the peptide in humans, Moscona wants to replicate these results in another animal model, such as mice.
Another nasal-spray compound, developed by Richard Leduc, a molecular pharmacologist at the University of Sherbrooke in Canada, and his colleagues is a small molecule that inhibits a host enzyme needed by viral particles to fuse with a target cell. Leduc and his colleagues found that mice given nasal doses of the compound became infected with the coronavirus, but they had much less virus in their lungs than did mice that received only saline2. Leduc and his colleagues are working to increase the peptide’s effectiveness by making it more stable and selective before moving on to testing it humans. Both Leduc and Moscona are working with companies to bring their products to market.
The runny-nose challenge
Even if researchers find an antiviral compound that can be delivered as a nasal spray and prevents coronavirus infections in humans, they still face the challenge of ensuring that the compound stays in the nasal lining long enough to be consistently effective. “Your nose and throat are inherently designed to get rid of things,” Barclay says. “You try putting something in there, and your nose runs and flushes it out.”
Researchers could counteract this by designing the sprays to be reapplied more frequently, but Barclay cautions that the more often that people have to take a medicine, the less likely they are to adhere to the regimen. And even though the bulk of SARS-CoV-2 infections start in the nose, it might be necessary for a prophylactic to coat the mouth and throat and even the lungs, which would require delivery through a nebulizer.
Still, such a spray would be an important advance, especially in places where few people wear face masks, says Barclay. “If we had something which was invisible and you self-administered and it gave you confidence to keep going, I think it would be a real game-changer,” she says. “We could keep kids in school.”



