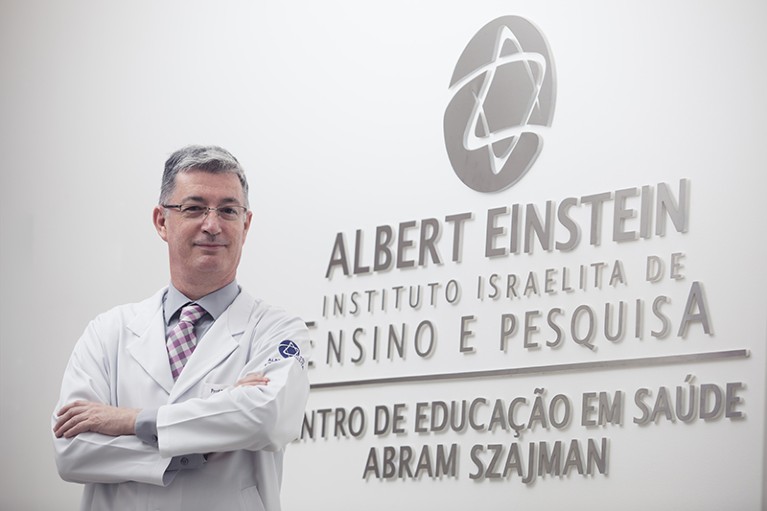
Luiz Vicente Rizzo is an immunologist and a research director at the Albert Einstein Israelite Hospital.Credit: Fabio H. Mendes/Albert Einstein
Luiz Vicente Rizzo is an immunologist and research director at the Teaching and Research Institute of the Albert Einstein Israelite Hospital in São Paulo, Brazil. Rizzo’s job is to coordinate all research activities across the Einstein, as the hospital is known among Brazilians. Rizzo spoke to Nature about how the Einstein spearheaded clinical studies during the COVID-19 pandemic, how science can improve patient care and what it means to coordinate research at one of the leading hospitals in Latin America.
How does a hospital’s research relate to its quality of care?
Doctors who do research keep up to date with what’s new in their field. As a consequence, they can offer the most modern treatments, even if not yet widely available.
Whatever kind of clinical research you do, taking something from the laboratory bench to the bedside and evaluating the outcome helps you to understand the populations you serve, including what works and what doesn’t. You will be able to improve care and even predict costs more accurately — which is important for both public and private health systems.
There’s another aspect that’s been known for years. Participants in studies generally have regular check-ups, someone who calls them to check that they’re taking their medication and are having all the appropriate tests done. That reduces their chances of missing doctors’ visits, or skipping a dose or being unable to access the medicine. Research patients are cared for with the greatest possible attention — that’s what the collection of data requires.
What research has your institute been leading?
We are one of the first hospitals in Latin America to be authorized to do research with CAR-T-cell therapy. This treatment is used mainly for leukaemia and lymphoma, and involves taking a patient’s T cells and modifying them by genetic engineering to get them to accept a receptor that recognizes a tumour antigen that the person has. The modified cells are then injected back into the individual so that their own immune system can fight the cancer. We are also about to start a trial using CRISPR gene editing to treat two genetic diseases with a high prevalence in Brazil: sickle-cell anaemia and epidermolysis bullosa, a condition in which the skin blisters easily.
How else does the Einstein’s research directly benefit patients?
We do a lot of nursing research. Our staff members, in both our public and private units, follow specific hand-washing protocols. It sounds trivial, but washing your hands is no simple business, and these people are responsible for treating more than 2 million Brazilians a year. We’ve done several studies1,2 about the most efficient hand-washing techniques to prevent hospital infections.
Your institute has a scientific-integrity office that periodically evaluates researchers. How did that come about?
We set up the office because the number of papers we published started to increase rapidly. Last year, we published almost 1,300 papers. That greatly increases the chance of mistakes, so we needed to find a way to catch those.
But we didn’t want to create witch hunts: the fact that you make a mistake does not mean that you are a bad person or a bad scientist. So, we decided that we would look for problems before someone else told us about them.
Every month, our staff audits two or three research projects that have completed more than 50% of their data collection. The team evaluates whether safety considerations are being followed, whether the data are properly stored and whether results are reliable. It also audits two or three papers that were published in the past couple of years. Researchers must provide all the raw data for these audits.
We believe that scientific integrity should be monitored for educational purposes, and not be seen as policing. The goal is not to catch researchers doing things wrongly, but to teach them the right way to do them.
How does your institute approach research management?
We have a small group of researchers: about 100. So we need to manage equipment, software and facilities to multiply what those researchers do.
We have found that sharing research space is very effective in promoting multidisciplinary research. When people in immunology, cardiology and neurology share space and equipment, they talk. And when they talk, they think up research that is multidisciplinary and, often, receives more funding than does non-multidisciplinary work and is published in better journals.
When we introduced this system, about 14 years ago, only 10% of our research involved multiple departments. Today, 100% of it does.
This interview has been edited for length and clarity.
This article is part of Nature Spotlight: Research hospitals, an editorially independent supplement. Advertisers have no influence over the content.

