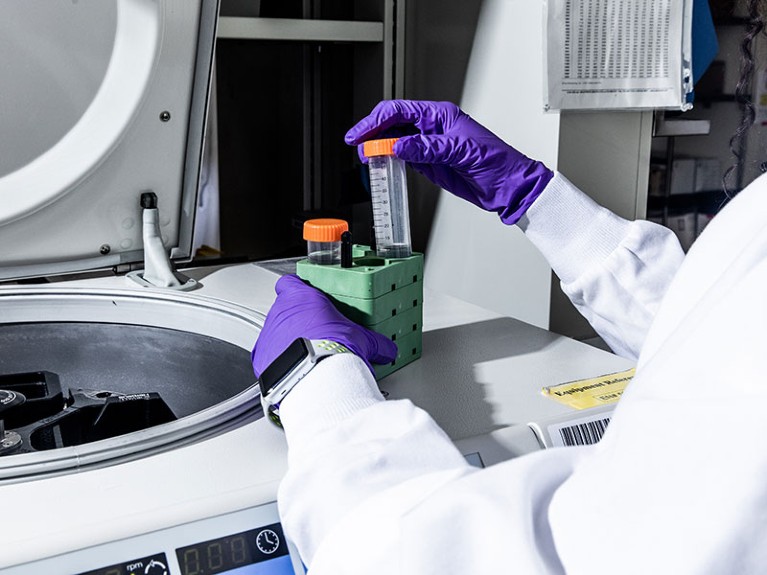
Lab assistants working at Amgen, a pharmaceutical company that is testing one of its cancer drugs at lower doses.Credit: Roger Kisby/Redux/eyevine
Chemotherapies aim to destroy as many cancer cells as possible, so drug development is guided by a preference for high doses. The standard approach to clinical trials for cancer drugs is to increase the dose until one-third of the participants abandon the trial. Drug-makers typically select a dose just below this as the default level to enrol more participants.
This ‘maximum tolerated dose’ approach is now being challenged in the United States. Officials at the Oncology Center of Excellence (OCE), part of the US Food and Drug Administration (FDA), are becoming concerned that the side effects of some cancer drugs are so toxic that patients stop taking them, writing in a 2021 New England Journal of Medicine editorial1 that sometimes “less is more”.
That editorial followed the launch, earlier in 2021, of the OCE’s Project Optimus, which encourages drug companies to identify cancer drug doses that balance tolerability with efficacy. Around the same time, as part of its accelerated approval for the lung-cancer drug sotorasib, the FDA asked the pharmaceutical company Amgen to run an extra clinical trial at a lowered dose — 240 milligrams per day instead of 960 milligrams — with a view to making the lower dose the default. The FDA has asked for a report on the results of this study to be submitted by February 2023.
Nature Index 2022 Biomedical sciences
The agency is also beginning to steer some drug developers towards testing multiple doses, rather than just the maximum tolerated dose, when seeking product approval.
This change in strategy has been welcomed by campaigners, many of whom have cancer. “I never could have imagined the degree of success so quickly,” says Anne Loeser, who has metastatic breast cancer, and leads the advocacy organization The Right Dose. Loeser consults with the FDA about its dosing strategy and attributes the latest changes to a 2021 survey carried out by her organization.
Presenting the survey results in June 2021 at the annual meeting of the American Society of Clinical Oncology, Loeser revealed that 86% of 1,200 respondents reported side effects such as nausea, fatigue or low blood cell counts, and almost half of respondents missed at least one treatment as a result. The survey also found that more than 83% of metastatic breast cancer patients felt better when their drug dosage was reduced.
Emerging cancer therapies are increasingly more targeted in their nature. Some are also designed to prime the patient’s own immune system to resist cancer’s spread. In this context, it’s especially sensible for drug developers to test at multiple doses, says Mark Ratain, a medical oncologist at the University of Chicago, Illinois, who also advises the FDA. “If you’re telling the world that you have a spectacularly targeted drug, then the optimum dose is not the maximum dose.”
FDA officials have agreed, arguing that the maximum dose paradigm doesn’t make sense for newer generation therapies. They are currently developing oncology-specific guidance on how to test multiple dosages in a clinical trial.
Mirat Shah, a medical oncologist based at the FDA in Silver Spring, Maryland, and the clinical lead for Project Optimus, says that the need to revise and lower approved dosages, as could happen with Amgen’s sotorasib, will become the exception rather than the rule once the changes envisioned by Project Optimus become routine. Ratain says that the emerging data from Amgen show that, for most patients, the lower dose will yield as many therapeutic benefits as the currently approved higher dose, with fewer side effects.
For now, OCE leaders have not yet issued any formal guidance on how drug developers should test different drug doses and the timeline for doing so is unclear. In the meantime, some established FDA guidance about balancing tolerability with efficacy, some of which dates to the 1990s, could be helpful to pharmaceutical companies. In a webinar from September 2022 about Project Optimus, speakers from the health-care consultancy Paraxel in Durham, North Carolina, pointed to these guidance documents and offered advice for drug developers about how to prepare for the FDA’s emerging era of oncology-drug development.
Loeser is optimistic that change is coming. “This is really addressing the root cause of so much suffering among oncology patients,” she says.